Abstract
Background: Air-leak syndrome (ALS) occurs when there is leakage of gas from the alveoli, which results in clinical symptoms including cough and sputum, dyspnea, and hypoxemia. ALS is rare but potentially life-threatening in patients who have received an allogeneic hematopoietic stem cell transplantation (allo-HSCT) and is an independent prognosis factor of patients undergoing HSCT. However, the clinical features and risk factors for post-transplant ALS among pediatric patients have rarely been explored.
Aims: This study analyzed the clinical characteristics, risk factors, clinical treatment options and prognosis to provide a scientific basis for ALS prevention and treatment for pediatric patients.
Methods: We retrospectively reviewed patients who were diagnosed with ALS following allo-HSCT between January 2013 and December 2019 at the Hebei Yanda Lu Daopei Hospital, and analyzed the role of ALS in the prognosis of the HSCT.
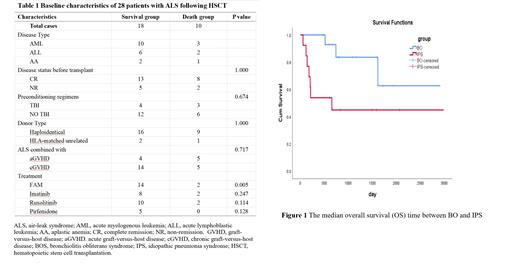
Results: A total of 2026 pediatric patients received an HSCT between January 2013 and December 2019. The ALS incidence rate was 1.4% (28 of 2,206 patients) with a survival rate of 64.3% (10 of 28 patients). The median overall survival (OS) time was 429 days (range: 55-1614 days). Sixteen patients were males and 12 were female. The median patients age was 12 years old (range: 1-16 years), and the median follow-up time was 871 days (range: 55-2973 days).We divided ALS into two categories: 15 cases of bronchiolitis obliterans syndrome (BOS) and 13 cases of idiopathic pneumonia syndrome (IPS). There was a significant difference in OS between the twogroups (80% among BOS patients versus 46% among IPS patients; P=0.037). Logical regression analysis showed that gender, an unmatched transplant donor and recipients (P=0.049), time to first occurrence of graft-versus-host disease after transplantation (P=0.021), and dosage of methylprednisolone >0.5mg/kg at the onset of ALS (P=0.049), were independent risk factors for poor prognosis in ALS. In addition, we found fluticasone, azithromycin, and montelukast (FAM) could significantly improve the prognosis following ALS (P=0.005). Compared with IPS, our results showed that some patients with BOS may benefit from imatinib (P=0.055), ruxolitinib (P=0.009), or pirfenidone (P=0.044).
Conclusion: ALS is a rare manifestation of pulmonary complications following HSCT among pediatric patients. Our analysis demonstrates that early diagnosis and FAM treatment may improve the survival rate of ALS following HSCT among pediatric patients.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal